 |
 |
- Search
| Precis Future Med > Volume 6(3); 2022 > Article |
|
Abstract
Fibromuscular dysplasia (FMD) is a noninflammatory and nonatherosclerotic disease that predominantly affects the renal and internal carotid arteries. However, the cause of this disease remains unclear. Radiological studies are important diagnostic methods, which generally involve luminal features on computed tomographic angiography, magnetic resonance angiography, and digital subtraction angiography. However, the high-resolution magnetic resonance imaging (HR-MRI) features of FMD have not yet been reported. Herein, we report the HR-MRI features of patients with FMD who showed typical involvement of the internal carotid arteries. Although both patients presented a beading appearance typical of medial fibroplasia, HR-MRI nevertheless showed distinct features. HR-MRI revealed concentric wall thickening and circular enhancement with dystrophic calcification in one and wall thickening, but no enhancement in the others. Further studies are required to determine whether these HR-MRI features are related to the type of FMD or patient prognosis.
Fibromuscular dysplasia (FMD) is a non-inflammatory and non-atherosclerotic disease of unknown cause which affects the small- and medium-sized arteries. The most commonly involved blood vessels are the renal and cervicocephalic arteries. If the disease involves the cervicocephalic arteries, it can cause abnormalities, including carotid and vertebral artery stenosis, arterial dissection, and aneurysm formation [1-3].
FMD is definitively diagnosed by imaging studies such as computed tomographic angiography (CTA), magnetic resonance angiography (MRA), and digital subtraction angiography (DSA) [2]. High-resolution magnetic resonance imaging (HR-MRI) techniques have recently been introduced to clinical practice, and provide a high value for the etiological diagnosis of intracranial arterial diseases [4-7]. Here, we report patients diagnosed with cervicocephalic FMD who underwent HR-MRI. To our knowledge, this is the first case report of HR-MRI in a patient with intracranial FMD.
A 60-year-old previously healthy woman was admitted with short-term vertigo lasting a few seconds. Vertigo was aggravated by positional changes and improved with bed rest. Initial neurological examination results were normal. She was diagnosed with benign paroxysmal positional vertigo as the cause of symptoms. Brain CTA showed multiple stenoses and dilatations with a string-of-beads appearance in the left internal carotid artery (ICA) (Fig. 1A). The patient was admitted to our hospital for DSA. In the left common carotid artery angiogram, vessel tortuosity and a string of beads were observed from the left petrous portion to the ICA bifurcation, a typical luminal feature of FMD (Fig. 1B). Aorta angiography revealed normal renal arteries bilaterally (Fig. 1C). HR-MRI revealed concentric wall thickening and saccular enhancement with dystrophic calcification in the distal segment of the left ICA (Fig. 2). Aspirin was prescribed at discharge, and she had no symptoms for up to 6 months after discharge.
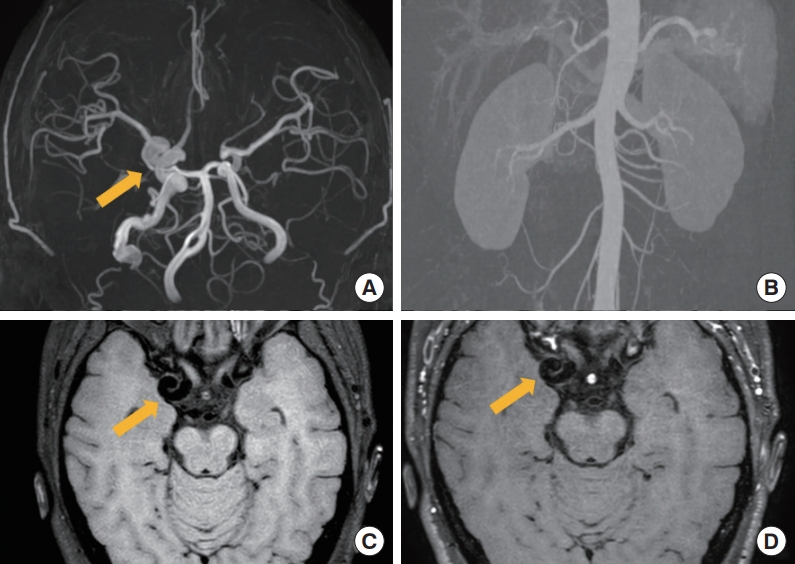
A 42-year-old, previously healthy woman visited our hospital with headache and shoulder pain. Initial neurological examination results were normal. She underwent brain MRI and MRA to rule out secondary headache. MRA of the brain further revealed dilatation and tortuosity of the right ICA (Fig. 3A). HR-MRI was performed for further evaluation, and aortic CTA was performed to identify any renal artery involvement. No stenosis or aneurysmal dilatation was observed in the renal arteries (Fig. 3B). HR-MRI revealed diffuse wall thickening but no enhancement in the right ICA from the petrous portion to the distal communicating segment (Fig. 3C, D).
Written informed consents by the patients were waived due to retrospective nature of our study.
Intracranial arteries are involved in 7% to 20% of cases of cervicoencephalic FMD [8]. Most cervico-encephalic FMD are located in the ICA, most commonly in the middle or distal segments. Vertebral artery involvement is less frequent and generally co-exists with carotid lesions. In addition, 50% of patients with carotid artery lesions have renal artery disease [9].
Our patient presented with headaches and vertigo. In the United States registry for FMD, 60% of patients experienced significant headache [10]. Pulsatile tinnitus is another common symptom of FMD. Dizziness may occur in one quarter of the patients, but true vertigo is uncommon in FMD. The most disruptive sequelae of cerebrovascular FMD include transient ischemic attack, stroke, subarachnoid hemorrhage, and cervical artery dissection, which have been reported in 13%, 10%, 1.1%, and 12% of patients, respectively [10]. Severe stenosis producing cerebral hypoperfusion, thromboembolism, dissection, and aneurysmal rupture could be mechanisms of focal neurological events. Treatment of FMD patients depends on the particular neurological symptoms and complications [8]. In this study, patients asymptomatic, and there were no vascular complications such as dissection and aneurysm.
The pathological classification of FMD is based on the dominant vessel wall layer, intima, media, and adventitia. Among the three pathological FMD types, the media type is the most common, accounting for more than 85% of cases [1,10,11]. Medial fibroplasia shows multifocal stenosis, termed the ‘string-of-beads; appearance, while intimal fibroplasia shows focal stenosis [3]. The cases presented in this report were classified as having media-type FMD involving intracranial ICA. Medial FMD presents as alternating areas of thinned media and thickened fibromuscular ridges in which the arterial muscle is replaced by fibroplasia with loose collagen [11].
In this series, HR-MRI of the first case showed concentric wall thickening and saccular enhancement, whereas the other case showed no enhancement. The clinical implications of vascular enhancement in FMD remain unclear. In cases with carotid web, also known as carotid intimal variant FMD, previous studies have shown that HR-MRI reveals protrusion with enhancement along the posterior margin of carotid bulb [12]. HR-MRI feature of concentric wall thickening may be related to the pathological features of thickened fibromuscular ridges. In addition, the HR-MRI findings of concentric enhancement with wall thickening in our case were similar to those of patients with symptomatic moyamoya disease [6]. Therefore, diffuse concentric enhancement within vessels could represent hyperproliferation of the vessel wall components and may be related to symptomatology in FMD. Further studies are needed to determine whether HR-MRI can provide information about the natural course of FMD.
In conclusion. HR-MRI can be used to directly visualize vessel walls. As the natural course of this disease varies among patients with FMD despite similarities in luminal features, further studies with HR-MRI are needed to test the diagnostic and prognostic role of HR-MRI in patients with FMD.
Notes
AUTHOR CONTRIBUTIONS
Conception or design: DGL, OYB, TKJ.
Acquisition, analysis, or interpretation of data: DGL, NJH, TKJ.
Drafting the work or revising: DGL.
Final approval of the manuscript: DGL, OYB, NJH, JC, TKJ.
Fig. 1.
(A) Brain computed tomographic angiography showing multiple stenosis and dilatation in the left internal carotid artery (arrow). (B) Digital subtraction angiography (DSA) shows vessel tortuosity and string-of-beads sign from the left petrous portion to the internal carotid artery bifurcation. (C) DSA showing bilateral normal renal artery at the renal-level aortogram.
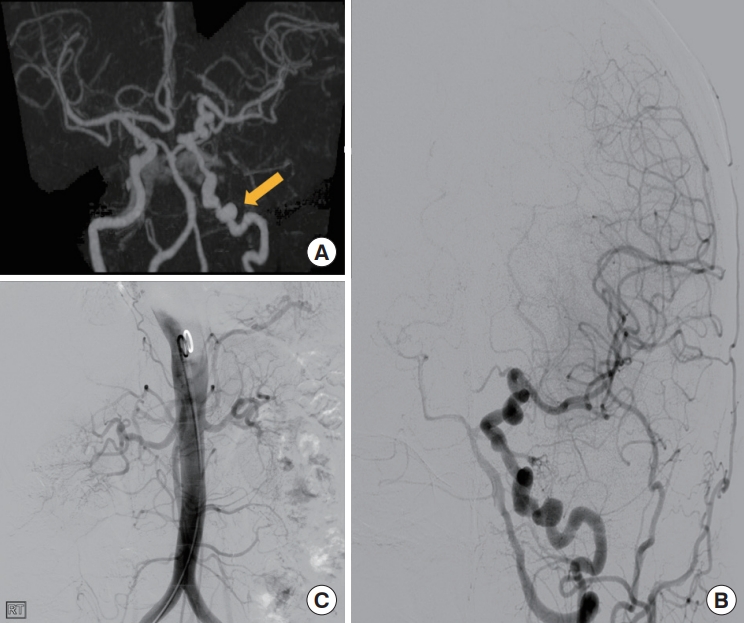
Fig. 2.
High-resolution magnetic resonance imaging showing concentric wall thickening and saccular enhancement with dystrophic calcification (arrows).
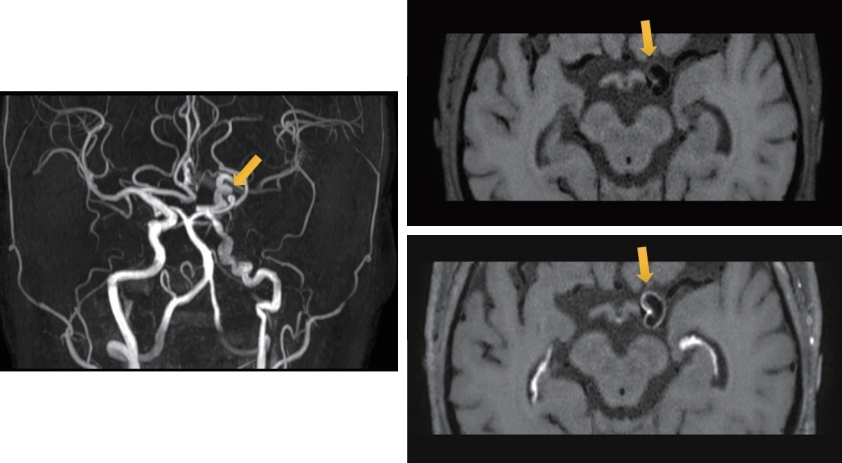
Fig. 3.
(A) Magnetic resonance angiography showing dilatation and tortuosity in the right internal carotid artery (arrow). (B) Aorta computed tomographic angiography showing no stenosis or dilatation. (C) Minimal wall thickening can be seen in the right internal carotid artery (ICA) in T1-weighted images (arrow). (D) No enhancement is visible in right ICA in T1-weighted contrast-enhanced images (arrow).
REFERENCES
1. Plouin PF, Perdu J, La Batide-Alanore A, Boutouyrie P, Gimenez-Roqueplo AP, Jeunemaitre X. Fibromuscular dysplasia. Orphanet J Rare Dis 2007;2:28.




3. Varennes L, Tahon F, Kastler A, Grand S, Thony F, Baguet JP, et al. Fibromuscular dysplasia: what the radiologist should know: a pictorial review. Insights Imaging 2015;6:295–307.




4. Bang OY, Toyoda K, Arenillas JF, Liu L, Kim JS. Intracranial large artery disease of non-atherosclerotic origin: recent progress and clinical implications. J Stroke 2018;20:208–17.




5. Sim JE, Park J, Bang OY. Non-thrombotic ischemic cerebrovascular events related to the use of tyrosine kinase inhibitors in patients with cancer: high-resolution magnetic resonance imaging findings. Precis Future Med 2021;5:199–203.


6. Ryoo S, Cha J, Kim SJ, Choi JW, Ki CS, Kim KH, et al. High-resolution magnetic resonance wall imaging findings of Moyamoya disease. Stroke 2014;45:2457–60.


7. Choi EH, Yu I, Park JH, Yoon CW, Bang OY. Reversible cerebral vasoconstriction syndrome without typical thunderclap headache: Highresolution magnetic resonance imaging features. Precis Future Med 2018;2:175–9.


8. Leary MC, Finley A, Caplan LR. Cerebrovascular complications of fibromuscular dysplasia. Curr Treat Options Cardiovasc Med 2004;6:237–48.



9. Touze E, Oppenheim C, Trystram D, Nokam G, Pasquini M, Alamowitch S, et al. Fibromuscular dysplasia of cervical and intracranial arteries. Int J Stroke 2010;5:296–305.



10. Olin JW, Froehlich J, Gu X, Bacharach JM, Eagle K, Gray BH, et al. The United States Registry for fibromuscular dysplasia: results in the first 447 patients. Circulation 2012;125:3182–90.









