 |
 |
- Search
| Precis Future Med > Volume 7(2); 2023 > Article |
|
Abstract
Purpose
We evaluated the clinical characteristics of patients undergoing cardiac magnetic resonance (CMR) examinations over 10 years at a tertiary referral hospital.
Methods
This retrospective study included 11,087 CMR examinations performed between November 2009 and September 2020. The number of adults aged ≥20 years was 10,648 (72.8% males). A total of 439 children or young adults aged < 20 years underwent CMR (66.5% males). Indications for CMR examinations were classified according to the Consensus Panel recommendations of the Society for Cardiovascular Magnetic Resonance (SCMR).
Results
The mean age was 55.9±12.4 years for adults. Forty percent of patients were obese. Leading cardiovascular risk factors were hypertension, dyslipidemia, diabetes mellitus, and current smoking status in 28.2%, 19.1%, 13.8%, and 25.4% of patients, respectively. The proportion of stress CMR examinations performed was 57.2%. For children, the mean age was 12.6±5.3 years. Most children underwent a non-stress CMR test. In adults without congenital heart disease, indication numbers for SCMR classes were 5,682 for class I (49.4%), 772 for class II (6.7%), 313 for class III (0.3%), and 4,714 for investigational group (41.1%). In pediatric patients and adults with congenital heart disease, indication numbers for SCMR classes were 539 for class I (80.3%), 62 for class II (9.2%), and 70 for the investigational group (10.4%).
Cardiac magnetic resonance (CMR) imaging has facilitated the diagnosis of various heart diseases [1,2]. Recent CMR techniques enable improved myocardial tissue characterization and quantification of flow in the cardiovascular system [3]. Deep-learning-based image reconstruction and analysis algorithms facilitate CMR examination and interpretation with high reliability [4]. However, despite the versatility of the imaging modality, the use of CMR in real-world practice has not been well appreciated [5].
Although requests for the use of CMR in clinical practice are increasing, prompt CMR examination and diagnosis may not be feasible in clinical scenarios. Therefore, a dedicated CMR unit is necessary to meet the needs of CMR examinations. In this study, we report the results of a dedicated CMR imaging center where over 10,000 cases of CMR were performed between November 2009 and September 2020. In this study, we aimed to evaluate the clinical characteristics of patients undergoing CMR examinations and indications of CMR for the past 10 years at a tertiary referral center.
From November 2009 to September 2020, 11,087 CMR imaging procedures were performed. Among them, the number of adults aged 20 years and over was 10,648 (96%; 7:3 = men: women). Of the 439 children who underwent CMR, two-thirds were male.
The magnetic resonance imaging (MRI) scanner used for the cardiac examinations was Siemens MAGNETOM Avanto1.5T (Siemens Healthineers, Erlangen, Germany). The types of CMR examinations were classified as either adenosine stress CMR or non-stress CMR. In adults, age was categorized as 20–29, 30–39, 40–49, 50–59, 60–69, and ≥70 years. And age was infant (0–0.9 years), toddler (1–2.9 years), preschooler (3–5.9 years), schooler (6–11.9 years), and adolescents (12–19.9 years). Body mass index (BMI) was calculated as the weight in kilograms divided by the square of the height in meters. Underweight and healthy weight were defined as a BMI < 23.0; overweight was defined as a 23.0≤ BMI < 25.0; obese was defined as a 25.0≤ BMI. We measured blood pressure, heart rate, and serum creatinine levels. The Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation was utilized to calculate the estimated glomerular filtration rate (eGFR) using as an indicator for kidney function. The equation is expressed as GFR= 141× min (serum Cr/κ, 1)α×max (serum Cr/κ, 1)-1.209×0.993age× 1.018 (if female), where κ represents 0.7 for females and 0.9 for males, α corresponds to –0.329 for females and –0.411 for males. The term ‘min’ denotes the minimum value between serum Cr/κ or 1, while ‘max’ indicates the maximum value between serum Cr/κ or 1. Chronic kidney disease (CKD) was defined as an eGFR below 60 mL/min/1.73 m2.
When CMR was performed, it was checked whether it was an outpatient department, in-patient department, emergency room, or health promotion center. We checked whether stress or non-stress CMR was performed. Indications for CMR examinations were classified according to the Consensus Panel recommendations of the Society for Cardiovascular Magnetic Resonance (SCMR) (Supplementary Table 1) [1].
We checked cardiac disease history, including myocardial infarction (MI), angina, cardiac catheterization, percutaneous transluminal coronary angioplasty (PTCA), PTCA stented, coronary artery bypass graft, congestive heart failure, atrial fibrillation/flutter, other arrhythmia, valvular heart disease, syncope, non-ischemic cardiomyopathy, myocarditis, congenital heart disease, congenital heart disease surgery, stress test including treadmill test and stress echocardiography, stress test results (negative, positive, equivocal, and incomplete exercise test), echocardiography, and others. Cardiovascular disease risk factors included hypertension, hypertension duration (years), hypercholesterolemia, family history of MI, family history of sudden death, diabetes, diabetes duration (years), renal disease, cerebrovascular accident/transient ischemic attack, aortic disease, and previous surgery or intervention. Patients who had engaged in smoking within the year preceding the study were classified as smokers.
The mean age of adult subjects was 55.9±12.4 years; 55.5± 11.7 years for men and 57.1±14.3 years for women (P< 0.05). Approximately 60% of all adults were in their 50s and 60s (Fig. 1). The proportion of male patients was 72.8%. The distribution of obesity was 42.5%. The mean systolic and diastolic blood pressure were 125.1±15.7 mm Hg in systolic and 71.7±15.7 mm Hg in diastolic blood pressure. The mean heart rate was 71.5±11.6 beats per minute. The proportion of CKD was 8.7%. The proportion of stress CMR examinations performed was 57.2%. The proportion of cardiac disease history was 8.7% for non-ischemic cardiac myopathy, 8.1% for MI, 2.8% for angina, 4.5% for heart failure, and 17.2% for arrhythmia, including atrial fibrillation and flutter. The proportions of cardiovascular risk factors were 28.2%, 19.1%, 13.8%, and 25.4% for hypertension, dyslipidemia, diabetes mellitus, and current smoking status, respectively (Table 1).
Of the 439 children who underwent CMR, two-thirds were male. Their mean age was 12.6± 5.28 years; 13.0± 5.17 years in boys and 11.8± 5.42 years in girls (P< 0.05). Approximately 90% of all children were 6 to 19.9 years old. Most patients underwent non-stress CMR tests (Table 2).
In adults without congenital heart disease, the number of indications for each SCMR class was 5,682 for class I (49.4%), 772 for class II (6.7%), 313 for class III (0.3%), and 4,714 for the investigational (41.1%) (Table 3, Fig. 2). In pediatric patients and adults with congenital heart disease, the number of indications for each SCMR class was 539 for class I (80.3%), 62 for class II (9.2%), and 70 for the investigational group (10.4%) (Table 4, Supplementary Fig. 1).
The number of yearly CMR examinations showed a decreasing tendency, probably because of the recent outbreak of epidemic infection with the Middle East respiratory syndrome virus in 2015. There were 1,346 in 2010, 1,154 in 2013, 738 in 2015, and 858 in 2019 (Fig. 3).
This study confirmed the clinical features and indications for CMR conducted at a tertiary medical center over a decade. Adult men were tested more frequently, and most were in their 50s or 60s. Stress CMR was performed in approximately 60% of cases. In adults without congenital heart diseases, the percentage of indications for each SCMR class was 49.4% for class I and 6.7% for class II. In pediatric patients or adults with congenital heart diseases, it was 80.3% for class I and 9.2% for class II.
It may be difficult to generalize the CMR indications in this study to other medical centers in this country or other countries. The CMR test is relatively expensive, costing approximately $700 to 900 in Korea. In United States, stress CMR can be a cost-effective gatekeeping modality in patients at risk for obstructive coronary artery disease (CAD) [6]. In a retrospective multicenter study of 2,340 patients, patients with chest pain syndrome without CMR ischemia or late gadolinium enhancement (LGE) experienced low annual rates of cardiac events (< 1%) and coronary revascularization (1% to 3%) and low spending on subsequent ischemia testing [7]. However, patients with ischemia and/or LGE experienced a > 4-fold higher annual primary outcome rate and a > 10-fold higher rate of coronary revascularization during the first year after CMR [7]. In Australia, stress CMR is the most cost-effective for the diagnosis of significant CAD, if exercise electrocardiogram stress testing is inconclusive or positive [8]. In the Stress Cardiac Magnetic Resonance Versus Computed Tomography Coronary Angiography for the Management of Symptomatic Revascularized Patients (STRATEGY) study comparing coronary computed tomography angiography (CCTA) and stress CMR, CCTA was associated with a higher rate of subsequent noninvasive tests (28% vs. 17%, P< 0.001), invasive coronary angiography (31% vs. 20%, P< 0.001), and revascularization procedures (24% vs. 16%, P= 0.007) and patients undergoing stress CMR showed a lower rate of major adverse cardiac events (5% vs. 10%, P < 0.010) and cost-effectiveness ratio (119.98 ± 250.92 Euro/year vs. 218.12± 298.45 Euro/year, P< 0.001) [9]. In an outcome-based study, CMR results helped avoid invasive procedures in 11% (38/361) of patients and prevented additional diagnostic studies in 7% (26/361) with per patient cost savings of $2,308 [10].
The use of CMR in health check-ups may be unique to this study. A randomized clinical trial showed that routine screening for CAD using coronary computed tomography angiography (CCTA) in patients with type 1 or type 2 diabetes did not reduce the composite rate of all-cause mortality, nonfatal MI, or unstable angina requiring hospitalization at 4 years [11]. A recent Danish trial also showed that population-based comprehensive cardiovascular screening using coronary artery calcium scores, ankle-brachial blood pressure measurements, and blood samples did not significantly reduce the incidence of death from any cause among men aged 65 to 74 years of age [12]. However, a systematic review and meta-analysis revealed that qualitative stress perfusion CMR has high accuracy for the diagnosis of CAD, irrespective of the reference standard and magnet strength [13] and the value of CMR in screening CAD with the capability of detecting physiologically significant CAD and MI has not been evaluated by randomized clinical trials. According to a CMR study in asymptomatic subjects, a combination of coronary magnetic resonance angiography (CMRA) with stress perfusion and delayed-enhancement MRI as a screening tool for the detection of CAD detected significant CADs in 13 (3.8%) of 341 subjects [14]. Among them, 11 subjects (3.2%) had both coronary artery stenosis (≥ 50% by diameter) on CMRA and stress perfusion defects in the corresponding areas. Five (1.5%) patients showed evidence of an old MI on LGE MRI. Three subjects (0.9%) underwent percutaneous coronary intervention after CAD had been detected on CMR. Normal stress perfusion and LGE MRI lead to excellent outcomes in predicting future cardiac events in asymptomatic subjects. Although CMR screening may be life-saving in a small number of asymptomatic patients, its application remains to be investigated.
In the United Kingdom (UK), there was a 5-fold increase in the number of CMR examinations over the last 10 years, with a 15% annual increase. However, access to CMR varies greatly across regions [5,15]. A recent UK survey [5] identified multiple indications for CMR, including cardiomyopathy (27%), stress perfusion (24%), function and viability (22%), heart failure (21%), myocarditis and/or pericardial disease (10%), pediatric and/or congenital heart disease (10%), acquired vascular disease (6%), valvular heart disease (5%), cardiac masses (3%), cardiac transplantation (0.4%), and others, with some overlap between indications. Another study conducted in a single center found that the most frequent indication for CMR was the assessment of myocarditis in 25.0% (650/2598) of cases, followed by adenosine stress perfusion (17.4%), assessment of impaired left ventricle (LV) function (14.2%), viability (6.6%), and aortic stenosis (4.3%) [16]. A report on the EuroCMR registry, which enrolled 27,000 consecutive patients, showed that the most common indications for CMR were risk stratification in suspected CAD and/or ischemia (34.2%), work-up of myocarditis and/or cardiomyopathies (32.2%), and assessment of viability (14.6%) [17]. In the Euro-CMR registry, CMR results led to a change in management in nearly 8.7% of cases [17].
For children, CMR is indicated for the assessment of aortic arch anomalies, pulmonary arteries, pulmonary veins, shunt lesions, tetralogy of Fallot, complex congenital heart diseases, single ventricle with palliative treatment, cardiac tumors, cardiomyopathies, coronary artery evaluation and myocardial perfusion [18]. Disease-specific protocols are used to evaluate congenital heart diseases [19]. The frequency of pediatric CMR use may vary across countries [20]. In Brazil, 52% of 142 sites rarely or never used CMR, and the main barriers to more frequent use of CMR were its high cost (65%), the need for sedation (60%), and an insufficient number of qualified professionals (55%) [20].
In Korea, the Ministry of Health and Welfare began to cover the fees in part for CMR examinations in patients with cardiomyopathy, complex congenital heart diseases, and anomalies of the great vessels in November 2019, which seemed to alleviate the burden of patients paying the cost for CMR examinations and increase patients’ opportunities for them. The availability of CMR scanners, due to the disparity between the needs of CMR scanning and the number of MRI equipment, also limits access to CMR scanning. In the UK, a country with high CMR activity levels and long waiting times (25 days in London and 180 days in Northern Ireland), it may be of clinical concern [5]. Considering the urgency of cardiovascular disease, dedicated CMR suites with a sufficient number of magnetic resonance scanners are highly desirable.
Recent technologies have broadened the diagnostic capabilities and indications of CMR, and in vivo depiction of myocardial tissue characteristics is feasible [21]. Fast CMR techniques such as compressed sensing (CS), optimized 3-dimensional cine and 4-dimensional flow, and fast strain-encoding imaging allow for rapid CMR examinations to improve patient workflow and reducing costs [22,23]. CS enables singlebreath-hold real-time cine imaging in daily practice and reduces scan duration 20 times without loss of clinical information [23]. In the CMR assessment of myocarditis, T1 and T2 quantifications are now recommended over T1-weighted and T2-weighted imaging, while LGE in a non-ischemic pattern remains in the updates of the 2009 Lake Louise criteria [24]. In coronavirus disease 2019 (COVID-19) patients, native T1, T2, post-contrast T1, and extracellular volume fraction calculation are desirable [25], as the common CMR findings of cardiac involvement in COVID-19 are mapping abnormalities and myocardial edema on T2-weighted images followed by LGE [26]. CMR feature-tracking techniques allow quantification of ventricular and atrial strain values from routine cine images and provide prognostic information in patients with various myocardial diseases [27]. Deep learning-based algorithms enable fully automated analysis of left ventricular function [28]. Machine learning impacts all aspects of CMR, including patient scheduling, data acquisition, image reconstruction, image quality improvement, image segmentation, quantification, and CMR reporting [4]. Radiomics may provide additional information on myocardial features compared with conventional techniques, and its benefits are still under investigation [29]. The recently developed four-dimensional flow technique can provide advanced hemodynamic measurements such as vorticity and helicity, wall shear stress, flow displacement, pressure gradients, viscous energy loss, and turbulent kinetic energy and will help in understanding the pathophysiological mechanisms of cardiovascular diseases [30]. Thus, continuing technical and clinical advances in CMR will change the classes of indications [1].
CMR was commonly performed in men in their 50s to 60s in this study. This finding might be explained by the fact that some diseases such as CAD and cardiomyopathy are more prevalent in men than in women [31-33]. It is also partly due to inclusion of stress CMR in the health promotion programs in our Health Promotion Center and in that case CMR was mostly performed in men aged 50 to 60 years.
Stress CMR was less commonly performed in patients with CAD than non-stress CMR, because most of them are diagnosed with stress echocardiography, coronary computed tomography, or cardiac catheterization. In patients with acute or chronic MI, myocardial viability and LV function were assessed with non-stress CMR. As our study was conducted in a single tertiary hospital in Korea, the findings from this study may not be generalized to other populations and clinical settings.
In conclusions, over the past decade, 10,648 adults underwent CMR, with 73% of them being men. The proportion of stress CMRs was 60%. CMR may be used as the first-line imaging technique (SCMR class I) in approximately half of adult patients and most pediatric patients.
Supplementary materials
Supplementary Table 1.
Classification of usefulness of cardiovascular MRI proposed by SCMR
Supplementary Fig. 1.
Distribution of the Society for Cardiovascular Magnetic Resonance (SCMR) by adults (11,481 cases) and children (671 cases). Children represent pediatric patients or adults with congenital heart diseases. Inv, investigational.
CONFLICTS OF INTEREST
Sung-Ji Park has been editorial board of Precision and Future Medicine since December 2017. She was not involved in the review process ofthis original article.
Notes
AUTHOR CONTRIBUTIONS
Conception or design: SYJ, YHC.
Acquisition, analysis, or interpretation of data: SYJ, JK, YSK, YAC, WJ, HOK, KY, EKK, SAC, SWP, DKK, SMK, JH, JS, ISK, SJC, JKO, SCL, YHC.
Drafting the work or revising: SYJ, EKK, SAC, SWP, DKK, SMK, JH, JS, ISK, SJC, JKO, SCL, YHC.
Final approval of the manuscript: SYJ, JK, YSK, YAC, WJ, HOK, KY, EKK, SAC, SJP, SWP, DKK, SMK, JH, JS, ISK, SJC, JKO, SCL, YHC.
Fig. 1.
Distribution of 11,087 patients for cardiac magnetic resonance examination by sex and age group.
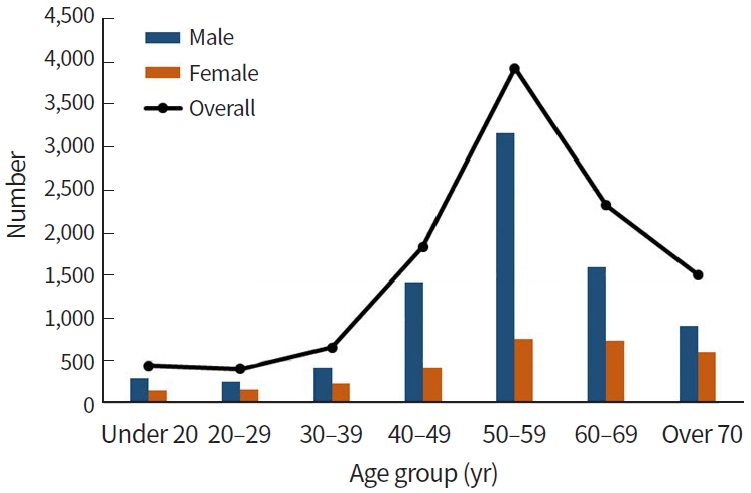
Fig. 2.
Acute myocarditis in a 36-year-old male. (A, B) Cardiac magnetic resonance shows a mild degree of myocardial enhancement (late gadolinium enhancement [LGE], arrows) in the mid-to-apical interventricular septum and lateral wall and focal enhancement in the inferior wall on LGE images. (C) Pre-contrast and (D) post-contrast (E) T1 mapping and T2 mapping in the middle myocardial segments showed abnormal values in the whole myocardium, including the lateral walls, which did not show remarkable LGE. The extracellular volume fraction was also abnormal (35.1%). An endomyocardial biopsy revealed interstitial lymphohistiocytic infiltration with some eosinophils and illdefined granulomas, consistent with myocarditis.
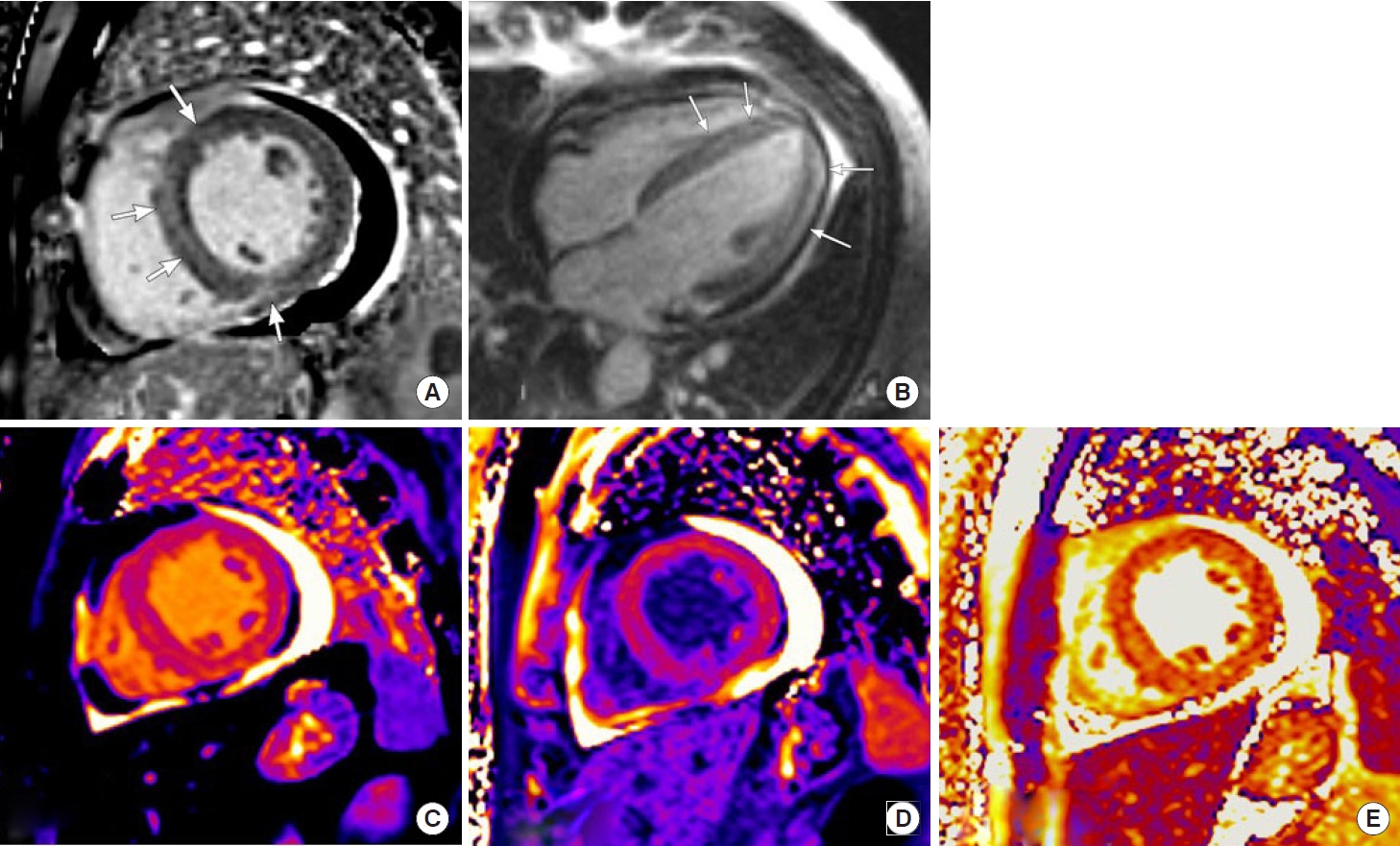
Fig. 3.
Distribution of patients with cardiac magnetic resonance examination from year 2010 to 2019.
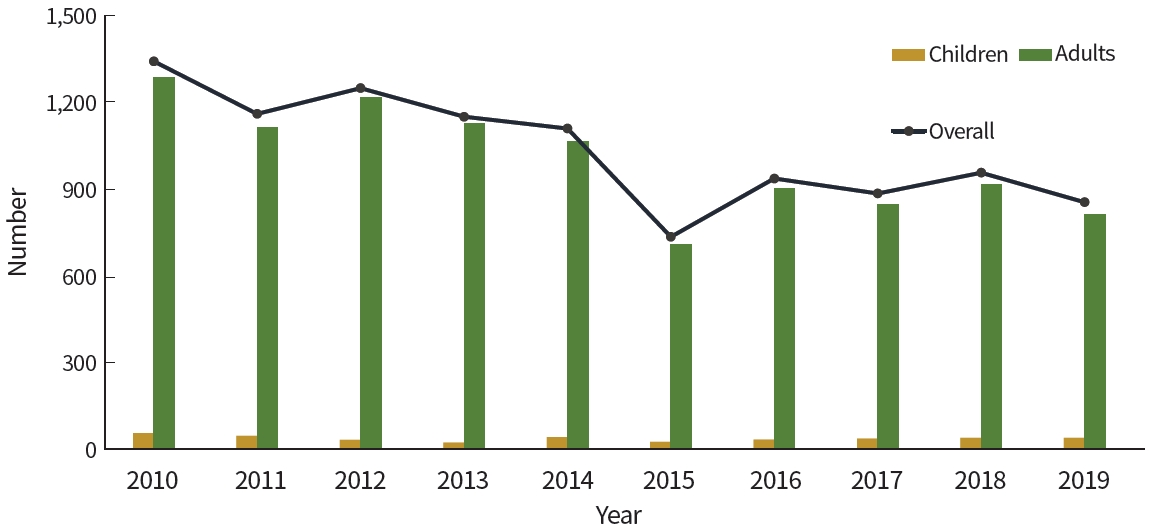
Table 1.
Distribution of clinical features, reason for scan, and risk factors for cardiovascular disease among adults who underwent a CMR imaging test
Table 2.
Distribution of clinical features for cardiovascular disease among children who underwent a CMR imaging test
Table 3.
Indications and classifications of CMR in adult patients in specific disease categories among 10,648 patients
Table 4.
Indications and classifications of CMR in patients in specific diseases categories among 439 children
REFERENCES
1. Leiner T, Bogaert J, Friedrich MG, Mohiaddin R, Muthurangu V, Myerson S, et al. SCMR Position Paper (2020) on clinical indications for cardiovascular magnetic resonance. J Cardiovasc Magn Reson 2020;22:76.




2. Busse A, Rajagopal R, Yucel S, Beller E, Oner A, Streckenbach F, et al. Cardiac MRI: update 2020. Radiologe 2020;60(Suppl 1):33–40.



3. Kim MY, Cho SJ, Kim HJ, Kim SM, Lee SC, Paek M, et al. T1 values and extracellular volume fraction in asymptomatic subjects: variations in left ventricular segments and correlation with cardiovascular risk factors. Sci Rep 2022;12:12544.




4. Leiner T, Rueckert D, Suinesiaputra A, Baeßler B, Nezafat R, Isgum I, et al. Machine learning in cardiovascular magnetic resonance: basic concepts and applications. J Cardiovasc Magn Reson 2019;21:61.




5. Keenan NG, Captur G, McCann GP, Berry C, Myerson SG, Fairbairn T, et al. Regional variation in cardiovascular magnetic resonance service delivery across the UK. Heart 2021;107:1974–9.



6. Ge Y, Pandya A, Steel K, Bingham S, Jerosch-Herold M, Chen YY, et al. Cost-effectiveness analysis of stress cardiovascular magnetic resonance imaging for stable chest pain syndromes. JACC Cardiovasc Imaging 2020;13:1505–17.


7. Kwong RY, Ge Y, Steel K, Bingham S, Abdullah S, Fujikura K, et al. Cardiac magnetic resonance stress perfusion imaging for evaluation of patients with chest pain. J Am Coll Cardiol 2019;74:1741–55.



8. Kozor R, Walker S, Parkinson B, Younger J, Hamilton-Craig C, Selvanayagam JB, et al. Cost-effectiveness of cardiovascular magnetic resonance in diagnosing coronary artery disease in the Australian Health Care System. Heart Lung Circ 2021;30:380–7.


9. Pontone G, Andreini D, Guaricci AI, Rota C, Guglielmo M, Mushtaq S, et al. The STRATEGY Study (stress cardiac magnetic resonance versus computed tomography coronary angiography for the management of symptomatic revascularized patients): resources and outcomes impact. Circ Cardiovasc Imaging 2016;9:e005171.

10. Hegde VA, Biederman RW, Mikolich JR. Cardiovascular magnetic resonance imaging-incremental value in a series of 361 patients demonstrating cost savings and clinical benefits: an outcome-based study. Clin Med Insights Cardiol 2017;11:1179546817710026.




11. Muhlestein JB, Lappe DL, Lima JA, Rosen BD, May HT, Knight S, et al. Effect of screening for coronary artery disease using CT angiography on mortality and cardiac events in high-risk patients with diabetes: the FACTOR-64 randomized clinical trial. JAMA 2014;312:2234–43.


12. Lindholt JS, Sogaard R, Rasmussen LM, Mejldal A, Lambrechtsen J, Steffensen FH, et al. Five-year outcomes of the Danish cardiovascular screening (DANCAVAS) trial. N Engl J Med 2022;387:1385–94.


13. Kiaos A, Tziatzios I, Hadjimiltiades S, Karvounis C, Karamitsos TD. Diagnostic performance of stress perfusion cardiac magnetic resonance for the detection of coronary artery disease: a systematic review and meta-analysis. Int J Cardiol 2018;252:229–33.

14. Song KD, Kim SM, Choe YH, Jung W, Lee SC, Chang SA, et al. Integrated cardiac magnetic resonance imaging with coronary magnetic resonance angiography, stress-perfusion, and delayed-enhancement imaging for the detection of occult coronary artery disease in asymptomatic individuals. Int J Cardiovasc Imaging 2015;31 Suppl 1:77–89.



15. Antony R, Daghem M, McCann GP, Daghem S, Moon J, Pennell DJ, et al. Cardiovascular magnetic resonance activity in the United Kingdom: a survey on behalf of the British Society of Cardiovascular Magnetic Resonance. J Cardiovasc Magn Reson 2011;13:57.




16. von Knobelsdorff-Brenkenhoff F, Bublak A, El-Mahmoud S, Wassmuth R, Opitz C, Schulz-Menger J. Single-centre survey of the application of cardiovascular magnetic resonance in clinical routine. Eur Heart J Cardiovasc Imaging 2013;14:62–8.


17. Bruder O, Wagner A, Lombardi M, Schwitter J, van Rossum A, Pilz G, et al. European Cardiovascular Magnetic Resonance (EuroCMR) registry: multi national results from 57 centers in 15 countries. J Cardiovasc Magn Reson 2013;15:9.




18. Valsangiacomo Buechel ER, Grosse-Wortmann L, Fratz S, Eichhorn J, Sarikouch S, Greil GF, et al. Indications for cardiovascular magnetic resonance in children with congenital and acquired heart disease: an expert consensus paper of the Imaging Working Group of the AEPC and the Cardiovascular Magnetic Resonance Section of the EACVI. Eur Heart J Cardiovasc Imaging 2015;16:281–97.


19. Fratz S, Chung T, Greil GF, Samyn MM, Taylor AM, Valsangiacomo Buechel ER, et al. Guidelines and protocols for cardiovascular magnetic resonance in children and adults with congenital heart disease: SCMR expert consensus group on congenital heart disease. J Cardiovasc Magn Reson 2013;15:51.




20. Kozak MF, Afiune JY, Grosse-Wortmann L. Current use of pediatric cardiac magnetic resonance imaging in Brazil. Arq Bras Cardiol 2021;116:305–12.


21. Kramer CM, Barkhausen J, Bucciarelli-Ducci C, Flamm SD, Kim RJ, Nagel E. Standardized cardiovascular magnetic resonance imaging (CMR) protocols: 2020 update. J Cardiovasc Magn Reson 2020;22:17.




22. Ibrahim EH, Frank L, Baruah D, Arpinar VE, Nencka AS, Koch KM, et al. Value CMR: towards a comprehensive, rapid, cost-effective cardiovascular magnetic resonance imaging. Int J Biomed Imaging 2021;2021:8851958.



23. Vermersch M, Longere B, Coisne A, Schmidt M, Forman C, Monnet A, et al. Compressed sensing real-time cine imaging for assessment of ventricular function, volumes and mass in clinical practice. Eur Radiol 2020;30:609–19.



24. Wheen P, Armstrong R, Daly CA. Recent advances in T1 and T2 mapping in the assessment of fulminant myocarditis by cardiac magnetic resonance. Curr Cardiol Rep 2020;22:47.



25. Kelle S, Bucciarelli-Ducci C, Judd RM, Kwong RY, Simonetti O, Plein S, et al. Society for Cardiovascular Magnetic Resonance (SCMR) recommended CMR protocols for scanning patients with active or convalescent phase COVID-19 infection. J Cardiovasc Magn Reson 2020;22:61.




26. Ojha V, Verma M, Pandey NN, Mani A, Malhi AS, Kumar S, et al. Cardiac magnetic resonance imaging in coronavirus disease 2019 (COVID-19): a systematic review of cardiac magnetic resonance imaging findings in 199 patients. J Thorac Imaging 2021;36:73–83.

27. Romano S, Judd RM, Kim RJ, Heitner JF, Shah DJ, Shenoy C, et al. Feature-tracking global longitudinal strain predicts mortality in patients with preserved ejection fraction: a multicenter study. JACC Cardiovasc Imaging 2020;13:940–7.

28. Kim YC, Kim KR, Choi K, Kim M, Chung Y, Choe YH. EVCMR: a tool for the quantitative evaluation and visualization of cardiac MRI data. Comput Biol Med 2019;111:103334.


29. Ma Q, Ma Y, Yu T, Sun Z, Hou Y. Radiomics of non-contrast-enhanced T1 mapping: diagnostic and predictive performance for myocardial injury in acute ST-segment-elevation myocardial infarction. Korean J Radiol 2021;22:535–46.




30. Strater A, Huber A, Rudolph J, Berndt M, Rasper M, Rummeny EJ, et al. 4D-flow MRI: technique and applications. Rofo 2018;190:1025–35.


31. Butters A, Lakdawala NK, Ingles J. Sex differences in hypertrophic cardiomyopathy: interaction with genetics and environment. Curr Heart Fail Rep 2021;18:264–73.











