|
 |
- Search
| Precis Future Med > Volume 7(2); 2023 > Article |
|
Abstract
Pheochromocytoma is one of recurrent tumors in patients with von Hippel-Lindau (VHL) disease. For patients with bilateral adrenal glands, unilateral adrenalectomy is the treatment of choice; however, for patients with a single adrenal gland, hemiadrenalectomy or tumorectomy can be performed instead of adrenalectomy to preserve adrenal function. Currently, adrenalectomy is recommended even if recurrent pheochromocytomas occur in the residual adrenal tissue. Consequently, adrenal insufficiency cannot be avoided in these patients. Percutaneous radiofrequency ablation (RFA) is used as an alternative treatment for preserving adrenal function; however, RFA is difficult to perform when major organs are present in the approaching pathway. The trans-hepatic approach is the only reported safe route to approach a right adrenal tumor to avoid pneumothorax. In this case report, we performed percutaneous RFA and hydrodissection through the left renal parenchyma to treat a recurrent pheochromocytoma in the small residual left adrenal tissue, which is surrounded by several critical organs. Our goal was to show our experience of image-guided trans-renal RFA and hydrodissection in a patient with VHL disease.
Adrenalectomy is the treatment of choice for sporadic unilateral adrenal tumors [1]. However, adrenal function cannot be preserved in the case of bilateral adrenal tumors. Accordingly, tumorectomy or hemiadrenalectomy is frequently recommended in patients with a history of unilateral adrenalectomy, to avoid adrenal insufficiency. Such cases occur in patients with hereditary pheochromocytomas associated with von Hippel-Lindau (VHL) disease or in multiple endocrine neoplasias [2].
Thermal ablation has been established as an alternative treatment for patients who are poor surgical candidates owing to a higher risk of postoperative morbidity or mortality. This minimally invasive treatment contributes to the preservation of adrenal function and the removal of adrenal tumors. A percutaneously accessible route is key to achieving successful ablation. Because the adrenal gland is surrounded by many critical organs such as the liver, spleen, kidney, gastrointestinal tract, pancreas, diaphragm, and major vessels, it is not always possible to approach adrenal tumors. The only safe and accessible pathway for adrenal biopsy or ablation is the trans-hepatic route to approach a right adrenal tumor to avoid lung injury [3-5]. To the best of our knowledge, there have been no reports on renal ablation procedures for adrenal tumors.
The purpose of this case report was to show our experience of computed tomography (CT)-guided trans-renal radiofrequency ablation (RFA) and hydrodissection for a recurrent pheochromocytoma in a patient with VHL disease.
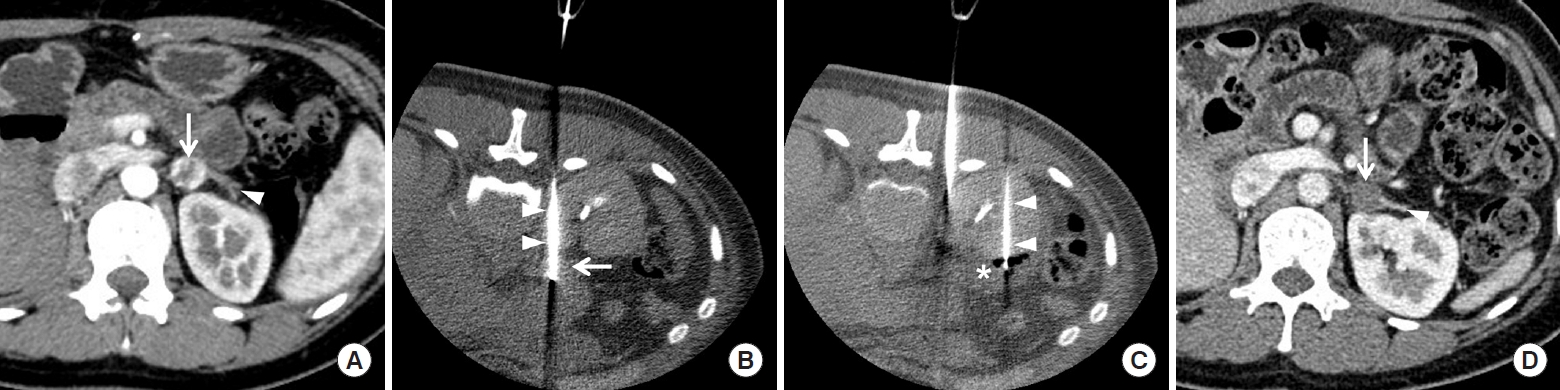
A 35-year-old woman was transferred to our hospital for treatment of recurrent pheochromocytoma. She had been diagnosed with VHL disease 10 years previously and undergone right adrenalectomy and left hemiadrenalectomy for recurrent pheochromocytoma. Recently, the patient presented with elevated levels of catecholamines in the urine and plasma; contrast-enhanced CT showed a recurrent pheochromocytoma in the residual left adrenal gland. Her endocrine clinician recommended adrenalectomy but decided to perform RFA to preserve adrenal function. Pre-ablation CT showed a small pheochromocytoma located in the medial portion of the residual left gland (Fig. 1A). The tumor measured 1.5 cm, was strongly enhanced, and was surrounded by the left kidney, jejunum, spleen, pancreas, diaphragm, and aorta.
An interventional radiologist, with 10 years of experience in percutaneous thermal ablation, introduced a 17-gauge RFA electrode (Proteus, STARmed) through the left renal parenchyma under CT guidance (Fig. 1B). Blood pressure was stable, including during tumor targeting by the electrode. A 20-gauge Chiba needle was introduced through the left renal parenchyma for hydrodissection (Fig. 1C). A total of 400 mL 5% dextrose water was intermittently instilled to displace the jejunum and pancreas from the pheochromocytoma. Blood pressure increased rapidly, suggesting a hypertensive crisis, immediately after the first ablation cycle; thus, beta- and alpha-blockers were intravenously injected to control blood pressure. When the radiofrequency (RF) electrode was withdrawn, the renal parenchyma was cauterized for approximately 20 seconds to minimize renal bleeding. The tumor was completely ablated without heat damage to the neighboring organs. The patient was discharged without signs or symptoms of adrenal insufficiency. The levels of urine and plasma catecholamines normalized post-RFA and follow-up CT showed no signs of residual or recurrent pheochromocytoma (Fig. 1D).
Approval of Institutional Review Board or informed consent was not necessary because of case report.
Trans-renal ablation and hydrodissection were technically successful in the present case without significant complications. The kidney is a hypervascular organ compared with other critical organs. Therefore, non-vascular interventions are rarely performed through the renal parenchyma; thus, there are few reports on trans-renal ablation procedures in the literature for treating adrenal tumors that are not percutaneously accessible. Additionally, trans-renal hydrodissection is a rare interventional procedure to displace neighboring organs from the adrenal tumor. The left adrenal gland is surrounded by several critical organs such as the kidney, spleen, pancreas, aorta, duodenum, jejunum, stomach, diaphragm, and lungs. Thus, mechanical or thermal injury to these organs should be avoided. Damage to the gastrointestinal tract during ablation can lead to serious complications, such as perforation, peritonitis, abscess, or sepsis [2,6]. An injured pancreas may develop acute pancreatitis, juice leakage, or abscess formation [7]. A perforated aorta can cause massive bleeding and sudden death [8]. An injured spleen may induce bleeding, which may be exacerbated if the splenic vessels are injured [9]. If the diaphragm is injured, various complications may occur such as chest pain, dyspnea, eventuation, or hernia [10]. Injured lungs may result in pneumonia, effusion, fistulas, or pneumothorax [2,6].
The adrenal gland is frequently located close to the anterior aspect of the upper pole of the kidney. If an RF electrode is introduced in a perpendicular direction from the back, it should pass through the renal parenchyma to target the adrenal tumor. A 17-gauge RF electrode may result in renal bleeding; however, electrocauterization may help reduce the amount of bleeding during electrode withdrawal. Trans-hepatic approaches are frequently used to target right adrenal tumors to avoid mechanical or thermal injury to other organs [3-5]. However, this technique cannot be applied to target left adrenal tumors; thus, in the present case, a trans-renal procedure had to be employed.
Pheochromocytomas tend to be recurrent and multifocal in patients with VHL disease. The treatment of choice is adrenalectomy, which results in adrenal insufficiency if bilateral. Therefore, thermal ablation can be used as an alternative treatment to increase steroid-free survival rates. Adrenal insufficiency typically occurs when more than 80% of the adrenal glands are destroyed. A multidisciplinary discussion is necessary among endocrinologists, surgeons, and radiologists in each case, to determine the appropriate treatment modality for patients with pheochromocytomas [2,6].
Trans-renal ablation procedures present several limitations. First, these ablation procedures are difficult to master; thus, an expert in these approaches is required to increase the chance of efficient tumor ablation. Careless manipulation of the electrode may increase bleeding during the procedure, leading to transfusion or embolization. Second, pre-ablation planning needs to be carefully performed to determine whether a trans-renal procedure is necessary. CT fluoroscopy helps interventional radiologists to precisely target adrenal tumors via the renal parenchyma. Third, premedication with beta- and alpha-blockers is necessary to reduce the likelihood of a hypertensive crisis [2,6]. These antihypertensive agents should be administered intravenously, immediately after blood pressure is elevated.
In conclusion, trans-renal ablation procedures can be invasive and should be carefully performed by an expert, in cases where this approaching route is the only option to reach the adrenal tumor. Minimizing manipulation and precise targeting are key techniques for achieving successful adrenal ablation without significant complications.
Notes
AUTHOR CONTRIBUTIONS
Conception or design: BKP.
Acquisition, analysis, or interpretation of data: BKP.
Drafting the work or revising: BKP.
Final approval of the manuscript: BKP.
Fig. 1.
A recurrent pheochromocytoma in a 35-year-old woman with von Hippel-Lindau disease. (A) Pre-radiofrequency ablation (RFA) computed tomography (CT) image shows a well-enhancing recurrent pheochromocytoma (white arrow) in the residual left adrenal gland (white arrowhead). (B) RFA CT image shows an RF electrode (white arrowheads), which targeted the tumor (white arrow) through the left renal parenchyma. The patient was prone on the CT table. (C) RFA CT image shows a Chiba needle (white arrowheads), introduced through the left renal parenchyma. A total of 400 mL 5% dextrose water (white asterisk) was instilled for hydrodissection, to displace the jejunum and pancreas from the tumor. (D) Five-month post-RFA CT image shows complete ablation of the pheochromocytoma (white arrow) in the small residual adrenal tissue (white arrowhead).
REFERENCES
1. Uludag M, Aygun N, Isgor A. Surgical indications and techniques for adrenalectomy. Sisli Etfal Hastan Tip Bul 2020;54:8–22.


2. Park BK, Fujimori M, Shen SH, Pua U. Asian conference on tumor ablation guidelines for adrenal tumor ablation. Endocrinol Metab (Seoul) 2021;36:553–63.



3. Park BK. Ultrasound-guided genitourinary interventions: principles and techniques. Ultrasonography 2017;36:336–48.




4. Park JJ, Park BK, Kim JH, Jeong BC, Kim CK. Salvage computed tomography-guided transhepatic radiofrequency ablation for unresected aldosteronoma of adrenohepatic fusion after adrenalectomy. Int J Urol 2016;23:102–4.


5. Park SY, Park BK, Kim CK. Sonographically guided transhepatic core biopsies of right renal and adrenal masses: safety and short-term follow-up. J Ultrasound Med 2013;32:2013–21.

6. Park BK. Percutaneous adrenal radiofrequency ablation: a short review for endocrinologists. Endocrinol Metab (Seoul) 2020;35:750–5.




7. Saccomandi P, Lapergola A, Longo F, Schena E, Quero G. Thermal ablation of pancreatic cancer: a systematic literature review of clinical practice and pre-clinical studies. Int J Hyperthermia 2018;35:398–418.


8. Schamroth Pravda N, Codner P, Vaknin Assa H, Hirsch R. Management of ascending aorta perforation during transseptal puncture for left atrial appendage closure: a case report. Eur Heart J Case Rep 2021;5:ytab154.