Strategies to enhance graft performance in cord blood transplantation
Article information
Abstract
Umbilical cord blood (CB) serves as one of the alternative donor sources for hematopoietic stem cell transplantation (HSCT) in those patients lacking a matched related donor. However, the relatively high incidence of engraftment failure and/or delayed engraftment following cord blood transplantation (CBT) has been a major obstacle against its success. The usage of two CB units has made CBT possible in adults when a single CB unit with an adequate cell number is lacking, but it failed to demonstrate any beneficial effect in children and adolescents. In recent years, unmanipulated haploidentical graft has been replacing CB owing to its rapid availability along with low incidence of acute and chronic graft-versus-host disease due to the usage of post-transplant cyclophosphamide. Given this situation, overcoming the engraftment related issues is crucial in order for CBT to remain a realistic alternative of allogeneic HSCT. This review discusses the engraftment-related issues in CBT and recent advances to overcome those, highlighting the role of conditioning, ex vivo CB stem cell expansion, and cotransplantation of mesenchymal stem/stromal cells.
INTRODUCTION
The first successful cord blood transplantation (CBT) dates back to 1988 when a boy with Fanconi anemia received cord blood (CB) from his human leukocyte antigen (HLA)-identical sibling [1]. This success proved the notion that hematopoietic stem cells (HSCs) residing in human CB is enough to repopulate human bone marrow following an immunoablative or myeloablative conditioning. This pioneering achievement was followed by the first successful CBT using unrelated CB, delivered from the New York Blood Center, in an adult with chronic myelogenous leukemia in 1996 [2]. Since then, over 700,000 CB units have been donated for public use, and tens of thousands of banked CB have been used for alternative donor hematopoietic stem cell transplantation (HSCT) in patients with various malignant and non-malignant disorders lacking a matched related or matched unrelated donor [3]. However, the limited cell dose in a CB unit has often led to delayed engraftment or failed primary engraftment resulting in high incidence of infectious complications and unacceptably high non-relapse mortality [4-8]. Nonetheless, due to the rapid availability and less stringent HLA matching requirements, CB has become a useful alternative HSC source for patients who need urgent allogeneic HSCT [9,10]. Typically, the rate of neutrophil engraftment after CBT is in the range of 70% to 90% with a significant delay compared to that after other types of HSCT [4,11]. In a previous report by Yoo et al. [12], the rates of neutrophil and platelet recovery were approximately 90% and 75%, respectively, with the overall survival rate of only 47.5% following CBT in Korean children and adolescents. Given that the delayed engraftment or primary engraftment failure has been the biggest hurdle to a successful CBT, strategies aiming at enhancing the graft performance are urgently needed in order for CBT to remain a realistic alternative of allogeneic HSCT.
Herein the engraftment-related issues in CBT and recent advances in promoting engraftment after CBT have been discussed. Undoubtedly, selecting the best available CB unit that is well matched and has an adequate number of cells is the most important strategy for a successful CBT. In addition, avoiding CB units where preformed host donor specific anti-HLA antibodies exist is also a common practice to prevent graft failure or delayed engraftment [13-15]. With these strategies having been repeatedly stressed numerously, other strategies aiming at enhancing engraftment will be highlighted, which include modifying conditioning regimens, ex vivo CB stem cell expansion, and cotransplantation of third party mesenchymal stem/stromal cells (MSCs). This review mainly focuses on pediatric recipients who are more likely to benefit from CBT, in the hope of implicating some of them in adults as well.
HAPLOIDENTICAL TRANSPLANTATION VERSUS CBT
According to the European Group for Blood and Marrow Transplantation (EBMT) activity survey report in 2017, the number of unrelated CBT has been decreasing while that of haploidentical transplantation has been rapidly increasing in recent years [16]. The situation is similar in Korea. In 2018, CBT accounted for only 3.9% of all alternative donor transplants in contrast to 34% in 2004 (data provided by the Korean Blood and Marrow Transplantation Nurses Society). On the contrary, haploidentical transplantation was seldom performed until the mid-2000s, but it accounted for 45.9% of all alternative donor transplants in 2018 in Korea (data provided by the Korean Blood and Marrow Transplantation Nurses Society). These trends are largely attributed to recent advances in haploidentical transplantation using post-transplant cyclophosphamide, which has proved effective in preventing severe graftversus-host disease (GVHD) without the need for ex vivo T-cell depletion [17-19]. In addition, a haploidentical donor is usually rapidly available, and an adequate cell number is guaranteed in most cases. According to a recent retrospective study by the Eurocord-EBMT, the rates of overall survival, leukemia-free survival, and GVHD-free/relapse-free survival (GRFS) were significantly lower after CBT than those after haploidentical transplantation in adult patients with leukemia [20]. A more recent prospective randomized study by Sanz et al. [21] also revealed lower rates of disease-free survival and GRFS in adult CB recipients. These findings explain the general preference of physicians for a haploidentical transplantation over a CBT in adults when a matched related or matched unrelated donor is lacking. However, the situation is somewhat different in children. According to recent studies including a meta-analysis, the outcome measures for the two transplant modalities for childhood leukemia were comparable [22,23]. Given that CBT has advantages such as a low rate of chronic GVHD and a greater graft-versus-leukemia/graft-versus-malignancy (GVL/GVM) effect compared to other transplant modalities [24,25], establishing effective strategies to overcome its current limitations is expected to revitalize the use of CB especially for pediatric patients.
CB ENGRAFTMENT AND SURVIVAL IN PEDIATRIC MALIGNANCY
In a recent Japanese nationwide retrospective study comparing the donor sources in childhood acute leukemia, both neutrophil and platelet recovery after unrelated CBT were significantly delayed compared to those after unrelated bone marrow transplantation (BMT) [26]. The cumulative incidences of neutrophil recovery after matched related BMT, unrelated BMT, and unrelated CBT were 100%, 96.8%, and 86.6%, respectively. The median time to neutrophil engraftment was 17 days for matched related BMT, 19 days for unrelated BMT, and 23 days for unrelated CBT. The cumulative incidences of platelet recovery by day 100 after HSCT were 98.1% for matched related BMT, 91.2% for unrelated BMT, and 83.4% for unrelated CBT. Nevertheless, the incidences of acute GVHD after unrelated BMT and CBT were quite similar, and the incidence of chronic GVHD after CBT was lower compared to that after unrelated BMT. More importantly, the overall and leukemia-free survival rates after HLA identical sibling BMT (74.8% and 69.6%), unrelated BMT (69.0% and 71.8%), and unrelated CBT (75.0% and 63.8%) were comparable. More recently, a multicenter retrospective analysis comparing the donor sources in childhood acute myeloid leukemia in Europe, Australia, and the United States also showed comparable relapse and survival rates in the recipients of matched sibling donor, matched unrelated donor, and single CB [27]. In this study, only double CBT had worse survival compared to matched sibling donor transplant (hazard ratio, 0.43; 95% confidence interval, 0.23 to 0.83; P=0.013), indicating a tendency toward a lower leukemia-free survival (hazard ratio, 0.56; 95% confidence interval, 0.3 to 1; P=0.058) and a higher non-relapse mortality (hazard ratio, 0.42; 95% confidence interval, 0.16 to 1.1; P=0.071). Notably, the median time to neutrophil engraftment was 17 days for matched sibling transplantation, 19 days for both matched unrelated transplantation (P=0.31) and single CBT (P=0.03), and 22 days for double CBT (P<0.001). By 60 days, the rates of neutrophil engraftment were similar for all cell sources (approximately 95%). However, CBT, whether single or double, showed an evident delay in platelet engraftment, and a substantial proportion of patients failed to achieve it. The inferiority of double CBT in that study is not very surprising since an earlier study already revealed no beneficial effect of double CBT in children and adolescents [28].
As noted in these studies, both neutrophil and platelet engraftment are delayed after CBT for childhood malignancy; the primary graft failure rate appears to be decreasing, while a substantial proportion of patients still fail to achieve platelet engraftment. Nevertheless, overall and leukemia-free survivals after pediatric CBT are generally comparable to those after matched unrelated donor transplantations, and it would be desirable to avoid double CBT unless the cell dose of a unit is unacceptable for transplantation.
In patients with malignant diseases, there are many factors affecting the survival rates other than engraftment (e.g., disease status at transplantation, aggressiveness of the underlying disease, comorbid conditions). Therefore, the effectiveness of engraftment promoting strategies to improve survival rates is relatively uncertain, especially considering a relatively lower rate of primary engraftment failure in recent years than that in the past. Nonetheless, there are substantial evidences regarding the positive impact of total body irradiation (TBI) on the outcome of CBT in both children and adults. Nakasone et al. [29] showed that the rate of neutrophil engraftment was almost 20% higher in adult CB recipients following TBI-based myeloablative conditioning compared to that without TBI. Eapen et al. [30] compared an antithymocyte globulin (ATG)-free TBI-based regimen, named TCF (12 Gy TBI, cyclophosphamide 120 mg/m2, fludarabine 75 mg/m2), with other regimens for childhood acute leukemia. The showed that TCF regimen, whether as part of a clinical trial or not, resulted in superior survival as compared to other non-trial chemotherapy- or TBI-based regimens, suggesting that a specific conditioning regimen could affect the outcome of CBT for childhood malignancy [30]. However, they failed to prove its positive impact on engraftment. In our institution, we have been using an ATG-free modified TCF regimen, containing 10 Gy TBI, for childhood acute leukemia over a decade. All patients were engrafted successfully using this regimen; notably, their event-free and overall survival reached to almost 80% (unpublished data).
The main reason for using ATG in conditioning is in vivo depletion of host T-cells in order to prevent graft rejection. However, due to its long half-life and highly variable exposure between individuals caused by variables influencing the pharmacokinetic profiles, it also affects graft T-cells to a variable degree and can have a negative impact on engraftment [31]. Although ATG has been associated with a lower incidence of GVHD, it also decreases GVL/GVM effect and delays immune reconstitution [32,33]. Therefore, reducing its dose or even omitting it may be a reasonable choice given that an adequate cell dose and fairly good HLA matching are ensured.
CB ENGRAFTMENT AND SURVIVAL IN NON-MALIGNANT DISORDERS
In patients with non-malignant disorders, engraftment issues have been more problematic and the outcomes of CBT in those patients have largely been dependent on successful engraftment [34-37]. Unlike patients with malignant diseases who unexceptionally receive repetitive cytotoxic and immunosuppressive chemotherapy prior to HSCT, most of those with non-malignant disorders are not exposed to such treatments before transplantation. Therefore, they are capable of exerting relatively stronger alloimmune response against the graft despite a conditioning using similar intensity. This is also true for patients with severe aplastic anemia (SAA) whose marrow cellularity has already decreased, thus requiring a less intensive conditioning regimen.
As mentioned earlier, the first successful CBT was performed using CB from a matched related sibling donor [1]. However, a matched related CB or a fully matched unrelated CB unit is hardly available in clinical settings. Therefore, CB is mostly unrelated and partially mismatched in real practice. Nevertheless, matched related CBT has highly been successful in treating acquired and inherited bone marrow failure syndromes (BMFS) [35,38]. According to a study by the Eurocord and EBMT including 20 patients with acquired BMFS and 97 with inherited BMFS who were treated with matched related CBT, the cumulative incidence of neutrophil recovery by day 60 was 84% for acquired BMFS and 90% for inherited BMFS resulting in >80% long-term survival rates [38]. In contrast, an earlier report by the Eurocord-Netcord and EBMT on the unrelated CBT in Fanconi anemia showed a disappointing outcome [34]. The neutrophil recovery rate by day 60 was only 60%, and the 3-year overall survival was 40%. In this study, patients who received a nucleated cell dose greater than 4.9×107 per kg of recipients’ body weight showed a superior survival rate to those with a lower cell dose, which suggested that a higher cell dose is needed for the non-malignant disorders than that required in malignant diseases (2.5–3 × 107/kg). In a subsequent report in 2011, the Eurocord and EBMT compared the related and unrelated CBT for hereditary BMFS except for Fanconi anemia [35]. The engraftment rate of unrelated CB was only 55%, and there was substantial difference in 3-year survival between related and unrelated CBT (95% vs. 61%), again proving the necessity of a higher cell dose in unrelated CBT for these non-malignant disorders. In a concurrent study by the Eurocord and EBMT reported on the unrelated CBT in SAA including mainly pediatric patients, the rates of neutrophil and platelet engraftment were only 51% and 37%, respectively, resulting in very poor overall survival of 38% [36]. According to this study, infection (38%) and poor graft performance (32%) were the predominant causes of death followed by GVHD (7%). In 2014, the Korean CB Registry data on the unrelated CBT for pediatric non-malignant disorders was published [37]. The neutrophil engraftment rate was 85% in patients with acquired SAA and only 37% in patients with inherited BMFS, leading to the overall survival of 54% in the former and 37% in the latter.
Because of consistent poor outcomes, CB has not been considered a good stem cell source for treating non-malignant disorders. However, a recent Japanese study showed that a certain conditioning regimen was capable of producing an excellent outcome of CBT in pediatric patients with SAA [39]. They omitted ATG and used low-dose TBI (2 Gy), fludarabine (125 to 175 mg/m2), and either cyclophosphamide (50 to 100 mg/kg) or melphalan (80 to 120 mg/m2) for the conditioning before transplantation. This combination led to 100% engraftment and survival in contrast to the poor engraftment and survival with other regimens. More recently, a French nationwide prospective study on the unrelated CBT in patients with idiopathic refractory SAA was published [40]. The eligibility criteria required one or two CB units, containing separately or together more than 4×107 frozen nucleated cells per kilogram of recipients’ body weight. Twenty-six young patients aged between 9 and 23 years were enrolled, and they received fludarabine (120 mg/m2), cyclophosphamide (120 mg/kg), low-dose TBI (2 Gy), and low-dose ATG (5 mg/kg). There were only three graft failures, and the 1-year survival rate was 89%. Recently, a Japanese retrospective study on the unrelated CBT with fludarabine (125 mg/m2), cyclophosphamide (120 mg/kg), and low dose TBI (4 Gy) without ATG in adults with SAA was reported [41]. Although there were only six patients, all patients were engrafted and survived with a lower cell dose (median, 2.9×107/kg; range, 2.2 to 4.6) than that used in the previous French study (median, 4.3×107/kg in single CBT; median, 3.0×107/kg in double CBT).
In 2013, we launched a new conditioning regimen for pediatric CB recipients with SAA in our institution by modifying the previous one; the doses of fludarabine (75 mg/m2) and cyclophosphamide (120 mg/kg) were reduced with the addition of 5 Gy TBI and omission of ATG in the modified conditioning regimen. All three patients achieved sustained neutrophil and platelet engraftment and survived with full donor chimerism. No patient developed severe acute or extensive chronic GVHD (unpublished data). Now, we offer upfront CBT to children and adolescents with SAA who lack a matched sibling or matched unrelated donor whenever a suitable CB unit is available.
Very recently, an interesting report prospectively testing the strategy of reduced intensity single CBT with optional cord-donor leucocyte infusion (DLI) for non-malignant disorders was published [42]. Forty-four children with various diseases, mostly inherited, were enrolled, and a single CB unit containing >3×107 frozen nucleated cells per kg of recipients’ body weight and >1.5×105 CD34+ cells per kg of recipients’ body weight was eligible for the transplantation. The conditioning regimen included alemtuzumab, hydroxyurea, fludarabine, melphalan, and thiotepa. Additionally, the individualized doses of alemtuzumab and hydroxyurea was chosen depending on the patient’s condition. Five percent of thawed CB cells was re-cryopreserved for possible DLI, which was actually performed in 20 patients with conditions such as life-threatening viral infection, mixed T-cell chimerism, and sluggish T-cell reconstitution. Surprisingly, all evaluable patients achieved both neutrophil and platelet engraftment, and the 5-year survival rate (85%) was excellent without an increase of GVHD.
In summary, despite the consistent poor outcome of unrelated CBT in inherited non-malignant disorders in the past, both engraftment and survival rates are likely to be further improved by optimizing the conditioning regimen with or without an appropriate post-transplant intervention as needed. In addition, although limited, recent reports demonstrate a remarkable improvement in the unrelated CBT in patients with acquired SAA using ATG-free conditioning regimens containing low-dose TBI, fludarabine, and cyclophosphamide or using a similar low-dose ATG-containing regimen.
EX VIVO EXPANSION OF CB STEM CELLS
Ex vivo expansion of CB stem cells is one of the most attractive strategies to enhance graft performance. A number of methods for ex vivo expansion, such as Notch-mediated expansion [43-45], MSC coculture [46,47], nicotinamide [48-50], StemRegenin-1 [51,52], copper chelation [53,54], chrysin [55], and UM171 [56,57], have been explored and some of them have already been tested in clinical trials (Table 1). Ideally, expanded stem cells should maintain their quality by inhibiting hematopoietic differentiation, have to be safe and feasible for clinical application, must result in enhanced engraftment, and ultimately should lead to an improved survival of the recipients.
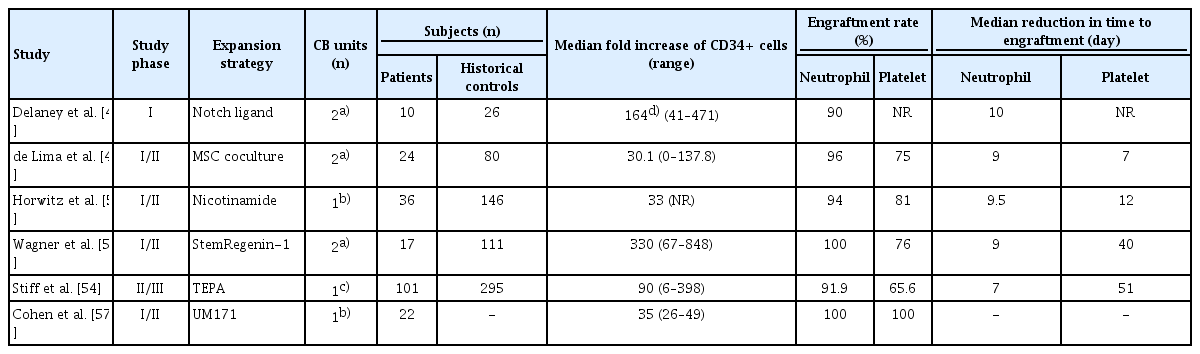
Overview of representative clinical studies on cord blood cells expanded ex vivo using small molecules or mesenchymal stem/stromal cell coculture
Notch family members are widespread by hematopoietic cells, and Notch signaling in combination with cytokines induces a robust increase in marrow repopulating ability of CB cells [43]. The first clinical trial with CB cells that have undergone Notch-mediated expansion was conducted in recipients of double CBT, and one of the two units was infused after ex vivo expansion [44]. The mean fold increase of nucleated cells was >500 times and that of CD34+ cells was >160 times, leading to a faster neutrophil engraftment compared to that in the historical controls (median reduction in time to neutrophil recovery, 10 days). This is the first report that demonstrated the rapid myeloid engraftment achieved using ex vivo expanded cells in human. The safety of Notch ligand-expanded progenitor cells was also demonstrated by a subsequent phase I study for patients with acute myeloid leukemia following intensive chemotherapy [45].
The first clinical trial using ex vivo expanded CB cells by MSC coculture was reported in 2012 [47]. Twenty-four recipients of double CBT received one unit CB cells expanded ex vivo in cocultures with stromal precursor antigen (STRO)-3+MSCs along with one unmanipulated unit. The median fold increases in nucleated cells and CD34+ cells were 12.2 and 30.1 times, respectively. This study also demonstrated improved engraftment kinetics in study subjects as compared to that in the historical controls, resulting in a median reduction in time to neutrophil recovery of 9 days (P<0.001) and a median reduction in time to platelet recovery of 7 days (P=0.03).
Nicotinamide is a small molecule which is known to inhibit the differentiation of hematopoietic stem and progenitor cells expanded by cytokine-induced ex vivo cultures and to enhance their functionality [48,49]. Recently, a phase I/II study assessing the safety and efficacy of CB grafts that were expanded ex vivo in the presence of nicotinamide and transplanted after myeloablative conditioning as a stand-alone graft was reported [50]. The expanded grafts showed 33-fold increase in CD34+ cells leading to a faster engraftment in the recipients of ex vivo expanded CB cells than that in the historical controls. The cumulative incidence of neutrophil engraftment was 94%, and the expanded grafts shortened the time to neutrophil (median, 9.5 days; P<0.001) and platelet (median, 12 days; P<0.001) recovery.
StemRegenin-1, an aryl hydrocarbon receptor antagonist, is a small molecule first identified in 2010 [51]. This promoted the expansion of CD34+ hematopoietic progenitor cells retaining their multi-lineage potential and significantly augmented the early and late engraftment of human cells in immunodeficient mice. A phase I/II study was performed in recipients of double CBT, they received one unmanipulated and one expanded unit of CB. CD34+ cells were expanded up to 848 times (median, 330; range, 67 to 848), leading to a substantially faster engraftment in the study subjects than that in the historical controls [52]. The marked expansion, absence of graft failure, and enhanced hematopoietic recovery supported testing of the StemRegenin-1-expanded single CB unit as a stand-alone graft.
Copper chelation by tetraethylenepentamine in combination with various cytokines inhibits stem cell differentiation transiently during the expansion period [53]. A cohort-controlled study using these expanded cells was recently reported [54]. Only a small portion of a CB unit was used for expansion in this trial, and the larger fraction containing nucleated cells at least greater than 1× 107/kg served as the unmanipulated fraction. The study presented an encouraging outcome showing a better engraftment kinetics and a significantly better 100-day survival in recipients as compared to that in the historical controls.
UM171, an HSC self-renewal agonist, has been shown to expand CB stem cells and enhance multi-lineage blood cell reconstitution in mice [56]. Very recently, a single-arm, phase I/II study of single UM171-expanded CBT was reported in patients with hematologic malignancies [57]. In this trial, no graft failure occurred in 22 patients who received single UM171-expanded CBT. The median time to neutrophil and platelet recovery was 18 and 42 days, respectively, without any unexpected adverse event.
As noted by a number of clinical trials, ex vivo CB expansion strategies are obviously encouraging in terms of facilitating engraftment following CBT. However, their impact on survival outcomes is uncertain due to the lack of large-scale long-term follow-up study on these measures. Further optimization of these strategies is expected to produce better outcomes of CBT in the near future.
COTRANSPLANTATION OF MSCS WITH CB
Cotransplantation of MSCs is another attractive investigational approach aiming at enhancing HSC engraftment. MSCs are known to play an important role in supporting hematopoiesis, and they also have immunomodulatory properties which enables them to suppress host allogeneic responses against the donor graft [58-60]. An early study showed that cotransplanted bone marrow-derived MSCs were able to promote the engraftment of CB CD34+ cells in sublethally irradiated non-obese diabetic/severe combined immunodeficiency (NOD/SCID) mice, and the effect was more prominent when the CB stem cell number was limited [61]. Previously, we demonstrated that the immunosuppressive abilities of MSCs are comparable with those derived from different sources including bone marrow, adipose tissue, CB, and Wharton-jelly [62]. More recently, we also showed that the engraftment promoting effect of MSCs is consistently observed regardless of the MSC source including bone marrow, adipose tissue, and CB [63]. Furthermore, we conducted a clinical trial using the third party CB-derived MSCs in pediatric CB recipients. All the patients cotransplanted with MSCs achieved both neutrophil and platelet engraftment faster than the historical controls [64]. However, in the past clinical trials on the cotransplantation of MSCs with CB, the engraftment promoting effect was not consistently observed. In a study by MacMillan et al. [65], all eight pediatric CB recipients cotransplanted with MSCs were successfully engrafted at a median of 19 days. However, a subsequent study by Gonzalo-Daganzo et al. [66] failed to demonstrate engraftment promoting effect of MSCs in adult recipients. This inconsistency might partly originate from the heterogeneity and/or limited functionality of MSCs in their naïve forms.
Next, it is interesting to see if certain techniques like preconditioning and genetic modifications could generate more potent and functionally augmented MSCs and if the functionally modified MSCs would be safe and more effective as well. Recently, we showed that MSCs preconditioned with interferon-γ significantly reduced the symptoms of GVHD in NOD/SCID mice, thereby increasing their survival rate when compared with naïve MSC-infused mice [67]. Upon interferon-γ-stimulation, a robust increase in indoleamine 2,3-dioxygenase (IDO) gene expression was observed. However, infusion of interferon-γ-primed MSCs in which IDO was downregulated did not elicit this effect, suggesting a pivotal role of IDO in the immunosuppressive function of MSCs. Importantly, these preconditioned MSCs and IDO-overexpressing MSCs showed similar survival of GVHD mice. In addition to interferon-γ-priming, culture density itself affects the gene expression profiles of MSCs. MSCs cultured at high density exhibited increased expression of various cytokine, chemokine, and growth factor genes involved in immunosuppression, migration, homing, angiogenesis, and reconstitution of damaged tissues [68]. These findings suggest that functional augmentation by means of certain measures can potentiate the innate abilities of MSCs including immunosuppressive and engraftment enhancing properties. Unlike other strategies aiming at enhancing graft performance, MSCs have also been useful in controlling steroid-refractory severe GVHD as shown in numerous previous studies [69-79]. Among them, a study by Auletta et al. [77] revealed the GVHD attenuating effect of MSCs without the loss of their GVL/GVM activity. However, MSCs have both anti-tumorigenic and pro-tumorigenic properties although they are not well established in hematologic malignancies (Fig. 1) [80]. Therefore, special precautions need to be taken while developing MSC-based cell therapies. Improving the quality of life as well as survival of recipients is the ultimate goal of HSCT. Thus, strategies aiming at controlling severe GVHD and preventing regimen-related toxicities and relapse are also as important as those aiming at facilitating engraftment in order to achieve the goal. Considering the safety and potential benefits of MSCs, the establishment of optimal treatment strategies with MSCs might pave the way for substantial improvement in the outcomes of not only CBT but also other types of allogeneic HSCT.

Mesenchymal stem/stromal cells (MSCs) exhibit a dual role in hematologic malignancy. They tend to not only inhibit tumor growth by suppressing tumor cell proliferation but also promote tumor growth by suppressing tumor cell apoptosis [80]. Adapted from Lee et al. [80], licensed under a Creative Commons Attribution 4.0 International (CC BY 4.0) License (https://creativecommons.org/licenses/by/4.0/).
CONCLUSION
Although a minority of pediatric CB recipients with hematologic malignancy suffer from primary graft failure, their survival appears to be comparable to that of haploidentical or matched unrelated donor recipients and even to that of matched related donor recipients in recent years. However, a delay in both myeloid and platelet engraftment is not likely to be overcome by double CB, which requires effective strategies to enhance engraftment. Engraftment failure has been especially problematic in CB recipients with non-malignant disorders. Nevertheless, recent data suggest that it can be overcome by modifying conditioning regimens with or without a specific post-transplant intervention. Thus, the optimization of conditioning regimens depending on the patients’ underlying disease might be the most practical and readily applicable approach along with selecting the best available CB unit to improve the outcome of CBT without an additional financial burden. There have been remarkable advances in ex vivo CB stem cell expansion technologies, and future clinical trials with a larger cohort will measure the effectiveness of these strategies. Despite some limitations of naïve MSCs in promoting CB graft performance, their innate immunosuppressive property is attractive enough to draw clinicians’ attention who are caring for patients under complicated post-transplant situations including severe GVHD. In this circumstance, further studies are needed to verify if functionally augmented MSCs would be able to help overcome the weaknesses of CBT.
Notes
No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTIONS
Conception or design: KHY.
Acquisition, analysis, or interpretation of data: KHY.
Drafting the work or revising: KHY.
Final approval of the manuscript: KHY.
Acknowledgements
This work was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (grant number: 2019R1A2C1084486) and by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI) funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI14C3484).
